Your Patient May NOT Need a Transfusion
Understanding Postural Pseudoanemia
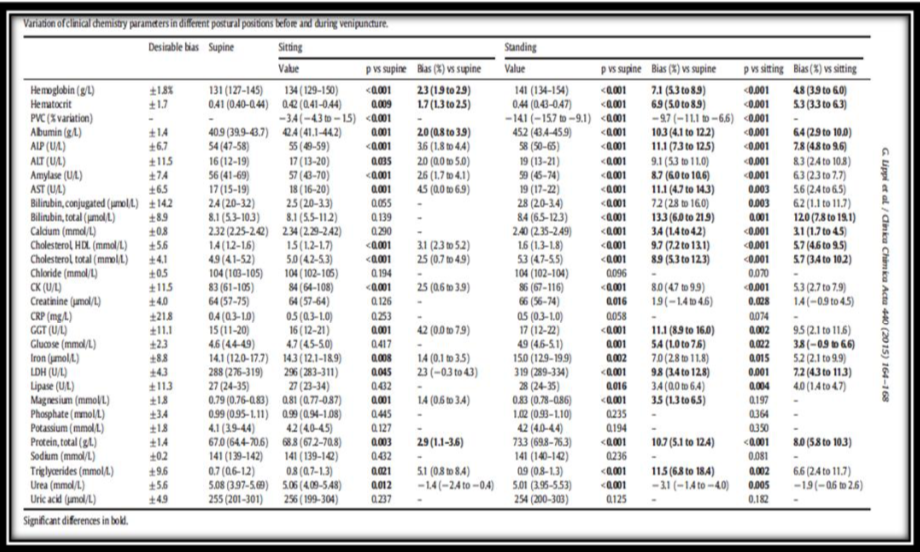
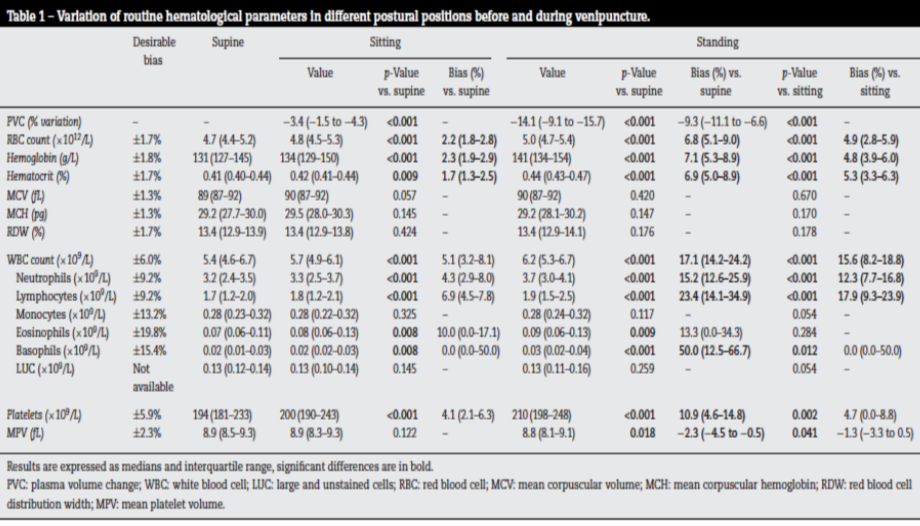
Simple changes in posture can cause wide fluctuations in hemoglobin (Hgb) and hematocrit (Hct), due to the redistribution of fluid between the intravascular and interstitial spaces. Plasma volume shifts significantly when a person changes position; after a postural change, restoration of equilibrium may take as long as 20 minutes(1). Standing up from a seated or supine position leads to rapid hemoconcentration as gravity causes blood to pool in the lower extremities, causing a hydrostatic shift of plasma fluid into the surrounding tissues. However, variations in lab values also occur with more moderate positional changes, such as going from sitting to a supine position. When a person is lying down, Hgb and Hct values can decrease by approximately 10%, as there is more volume in the intravascular space, leading to an apparent hemodilution. The changes occur in the fluid fraction and not in the red cell mass; therefore, the term postural pseudoanemia is used, as this state does not represent a true pathologic anemia.
A patent’s measured hematocrit may seem to have decreased significantly from a prior value, but this may simply be due to a change in the patient’s position between the two time points of the blood draw. This may alarm the physician, causing them to be concerned for acute anemia. They may then order an unnecessary ancillary tests as well as unnecessary blood transfusions. Therefore, it is important to understand when and how the phlebotomy occurred during each setting in order to better assess the need for a transfusion in a patient based largely on hemoglobin and hematocrit lab values, especially in the absence of other clinical signs or symptoms pointing to a need to transfuse.
Nurses and phlebotomists should aim to standardize patient position before venous blood collection, to minimize spurious lab test results. Because this may not always be possible, patient posture should be stabilized to one position for about 20 minutes before a blood draw. Physicians should take care to consider pre-analytical and other variables when receiving test results that do not match with the patient conditions, and communication between healthcare providers can help mitigate the alarm caused by unexpected laboratory findings.
Nurses and phlebotomists should include the following important parameters in their notes:
- Time of day the specimen was drawn
- The patient’s position
- Any other significant details related to the phlebotomy
References:
(1) Jacob G et al. Postural Pseudoanemia: Posture-Dependent Change in Hematocrit. Mayo Clin Proc. 2005. 80(5):611-614.
(2) Lippi G, et al. Postural change during venous blood collection is a major source of bias in clinical chemistry testing. Clinica Chimica Acta. 2015. 440: 164–168.
(3) Lima-Oliveira G et al. Patient posture for blood collection by venipuncture: recall for standardization after 28 years. Rev Bras Hematol Hemoter. 2017;3 9(2):127–132.
Katsikas 6/14/2018 NICL Laboratories, Ltd All Rights Reserved



 NICL Laboratories
NICL Laboratories